The amount of fluid (water) retained by
the body is controlled primarily by the kidneys. This occurs due to the
kidney's ability to control the retention and elimination of sodium and chloride, because the amounts of sodium, chloride, and
water in the body are carefully balanced. Thus, if sodium and chloride are
eliminated from the body, water also is eliminated. Conversely, if sodium and
chloride are retained by the body, so is water.
The elimination of
sodium, chloride, and water from the body is somewhat complex. In the kidneys,
sodium, chloride, and other small molecules are filtered out of the blood and
into the tubules of the kidney where urine is formed. Most of the sodium,
chloride, and water are reabsorbed into the blood before the filtered fluid
leaves the kidney in the form of urine. To make matters even more complex,
there are different mechanisms that are active in different parts of the
tubules that affect the reabsorption of
sodium and chloride.
A diuretic is any substance that promotes the production of urine. This includes forced diuresis. There are several categories of diuretics. All diuretics
increase the excretion of water from bodies, although
each class does so in a distinct way. Alternatively, an antidiuretic such as vasopressin, or antidiuretic hormone, is an agent or drug which reduces the excretion
of water in urine.
Uses of Diuretics
Diuretics are used with other types of
medications (adjunctive therapy) in edema associated with congestive heart
failure (CHF), cirrhosis of the liver,
and corticosteroid and estrogen therapy. Also are useful in
edema caused by renal dysfunction (for example, nephrotic
syndrome, acute glomerulo nephritis, and chronic renal failure).
Diuretics are used to lower urinary calcium
excretion, making them useful in preventing calcium-containing kidney
stones and as the sole therapeutic agents to treat hypertension. Diuretics can
also be used in combination with other antihypertensive drugs to
treat more severe forms of hypertension. Diuretics (specifically the carbonic
anhydrase inhibitors) are used as adjunctive treatment of chronic simple
(open-angle) glaucoma and secondary glaucoma
CLASSIFICATION
1. Acting at proximal convoluted tubules
1. Acting at proximal convoluted tubules
i. Osmotic
diuretics
· Glycerin,
Mannitole, Isosorbide and Urea
ii. Carbonic
anhydrase inhibitors
· Acetazolamide, Methazolamide
iii. Acidifying
drugs
· Ammonium chloride
iv. Others
like tea, coffee, Theophylline, etc.
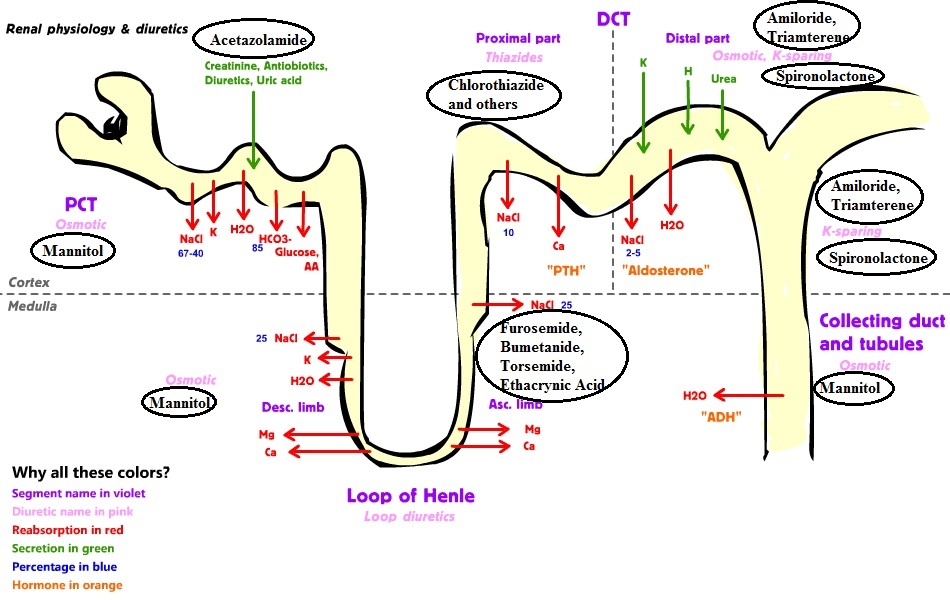
2.Acting at loop of Henle
i. Loop
diuretics
· Furosemide, Torsemide, Ethacrynic acid
ii. Mercurial
agents
· Mercaptomerin
3.Acting at distal convoluted tubule
i. Thiazides
diuretics
· Chlorothiazide, Chlorothalidone, Hydrochlorothiazide
ii. Sulfonamides
· Indapemide, Xipemide
4. Acting at collecting duct
system
i. K-
sparing diuretics
.
Aldosterone antagonist -
Spironolactone
.
Direct acting -
Triamterene,
Amiloride
ii. ADH antagonists
· Lithium salts, Demeclocycline
OTHERS
· Na/K acetate
· Na/K bicarbonate
· Na/K Acetate
· Albumin
· Dextrose
ANTI-DIURETICS
An
antidiuretic is an agent or drug that, when administered to an organism, helps
control body water balance by reducing urination opposing diuresis.Antidiuretics are the drugs that reduce urine volume, particularly in diabetes insipidus (DI) which is their primary indication.
Classification
1. Antidiuretic hormones - Vasopressin, also known as arginine vasopressin (AVP),
antidiuretic hormone (ADH), or argipressin, is aneurohypophysial hormone found
in most mammals. Its two primary functions are to retain water in the body and
to constrict blood vessels. Vasopressin regulates the body's retention of water
by acting to increase water reabsorption in the kidney's collecting ducts, the
tubules which receive the very dilute urine produced by the functional unit of
the kidney, the nephrons.
--ADH/Vasopressin, Desmopressin, Lypressin, Terlipressin
2. Miscellaneous
--Chlorpropamide, Carbamazepine
Sources--ADH/Vasopressin, Desmopressin, Lypressin, Terlipressin
2. Miscellaneous
--Chlorpropamide, Carbamazepine
Dale, M. M., H. P. Rang, and Maureen M. Dale. 2007. Rang &
Dale's pharmacology. [Edinburgh]: Churchill Livingstone.
Laurence L. Brunton (2011). Goodman &
Gilman's pharmacological basis of therapeutics. (12th
ed.). New York: McGraw-Hill.
http://www.rxlist.com/diuretics/drugs-condition.htm
https://en.wikipedia.org/wiki/Diuretic
https://en.wikipedia.org/wiki/Antidiuretic


